
The company had annual targets to reduce operational cost. Automating the process to send a prescription was one of the biggest opportunities that stood out.
I led the design for the project and my scrum team collaborated with a variety of stakeholders and departments including the care operations team, medical committee, patient experience teams and leadership.
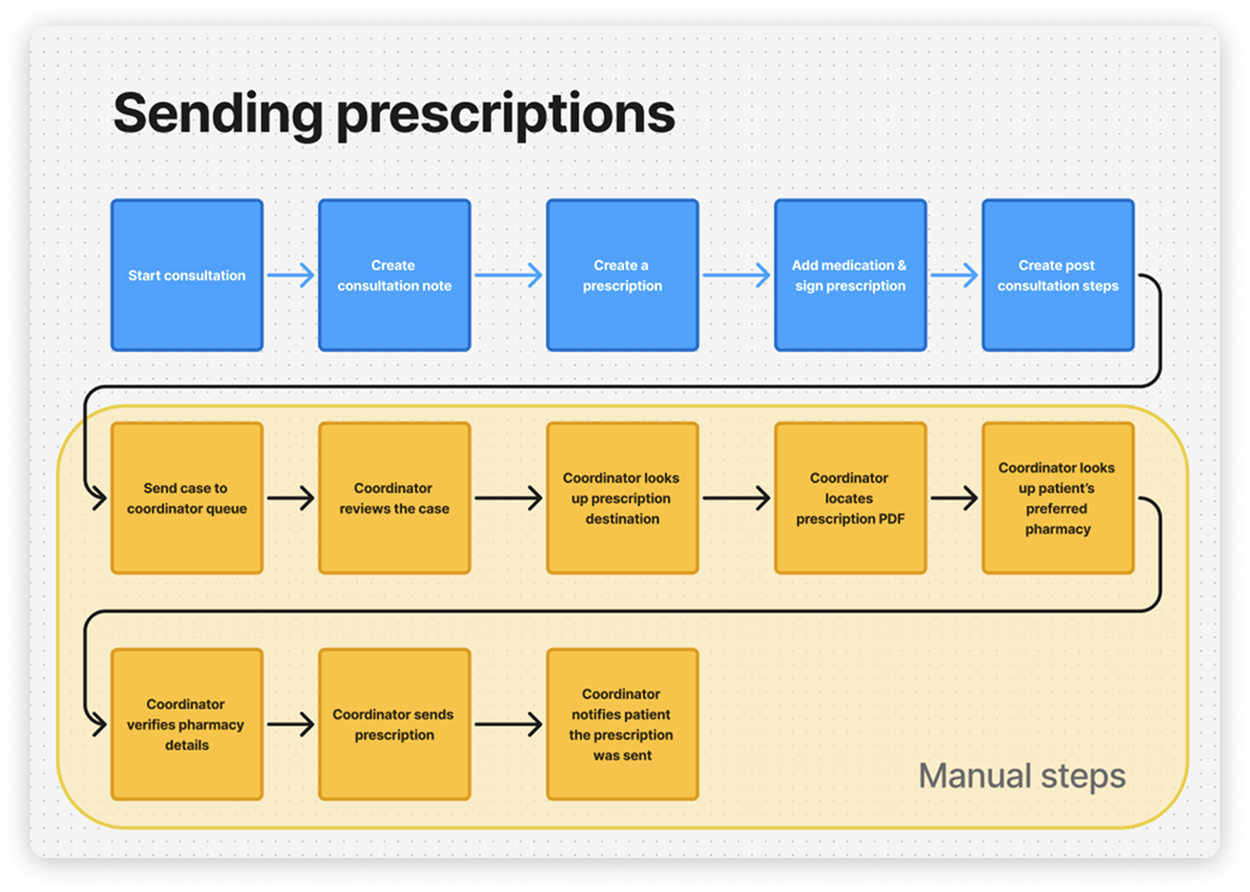
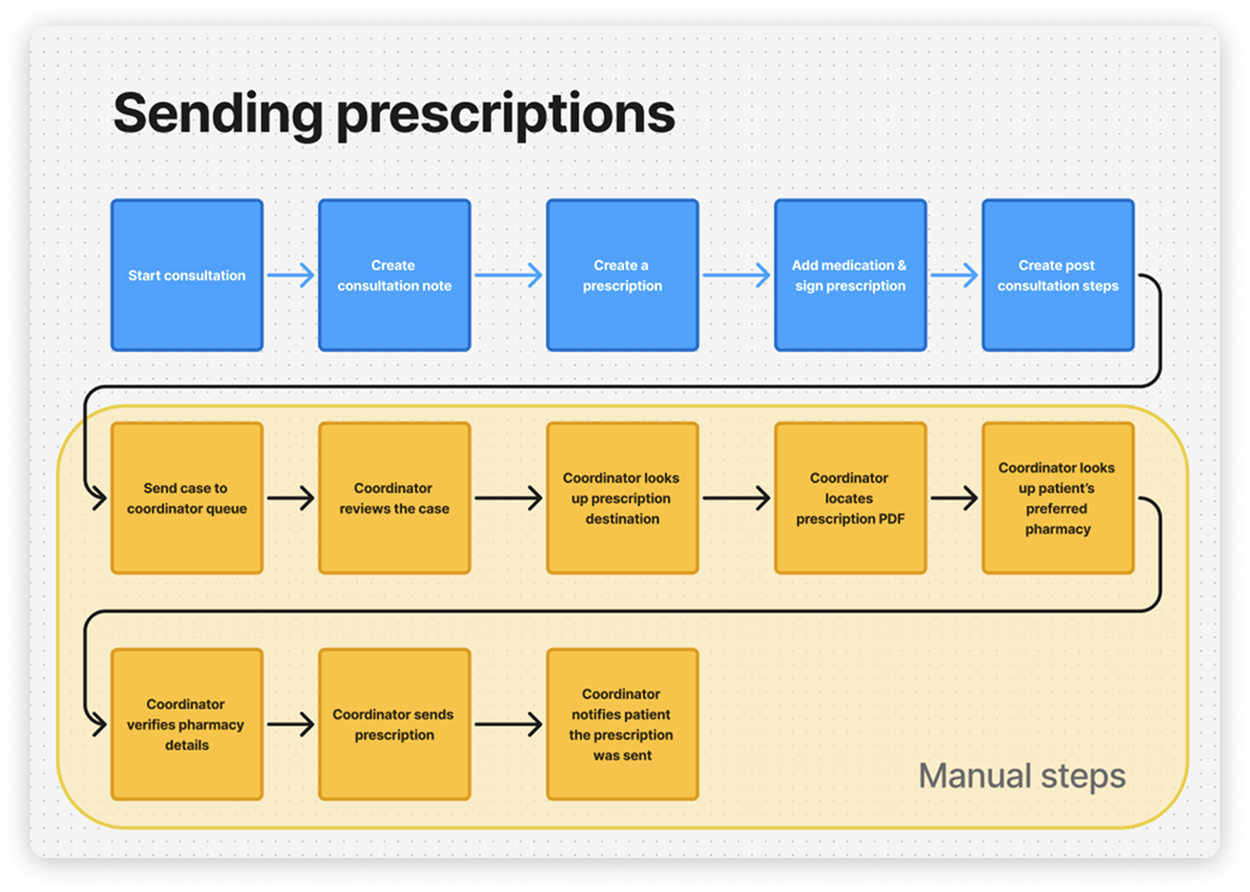
There were many steps in the process to send a prescription.
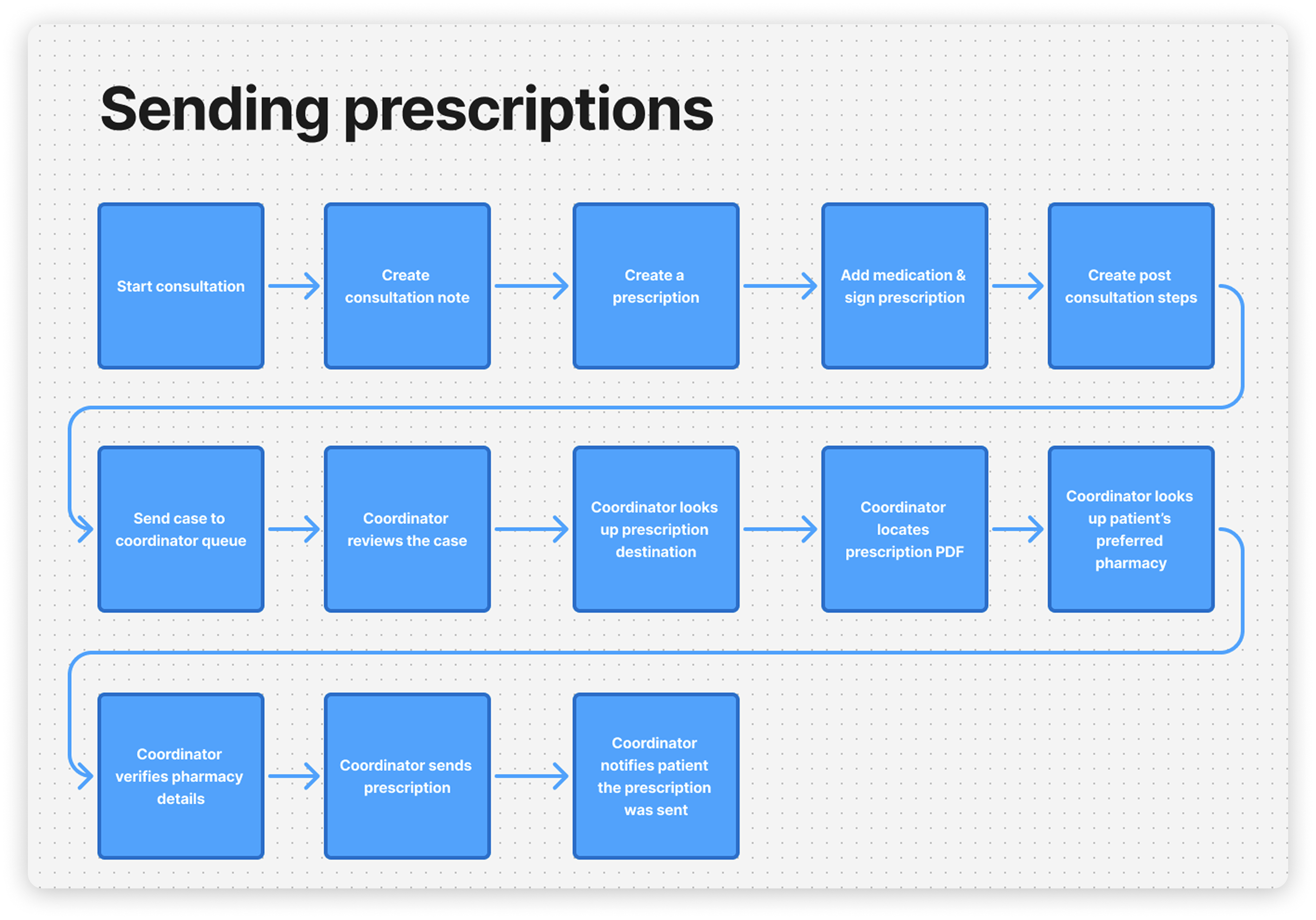
The vast majority of the steps were manual tedious tasks.
The vision was to provide the capability for every practitioner to send a prescription to a pharmacy right away.
The first barrier that stood in the way was resolving our system for managing pharmacies. The issues with the existing solution:
Most problems stemmed from a single failure point: untrustworthy data. Since the care team couldn't trust the information, they had to manually verify the information every time a prescription was sent.
I decided a few key principles were essential for the project:
The solution incorporated Google place IDs to ensure the starting point for each record was a legitimate business address. Afterwards, we built systems that could add more high quality information to the record. I decided a few key principles were essential for the project:

Surprisingly, the most challenging piece of information to gather was fax numbers. Prescriptions are unfortunately still sent through fax across Canada.
I created multiple prototypes to test the flow. I started with Figma at first and then took the opportunity to experiment with new AI prototyping tools. I used v0 for the majority of the time.

It also took a few iterations to figure out how we wanted to display the pharmacy record.

Through testing with the care team, the main features that improved the trustworthiness of the data were verification statuses and clearly indicating how the address information was sourced.
The pharmacy record had a few different views:



Examples of how it would be found within a patient's case:
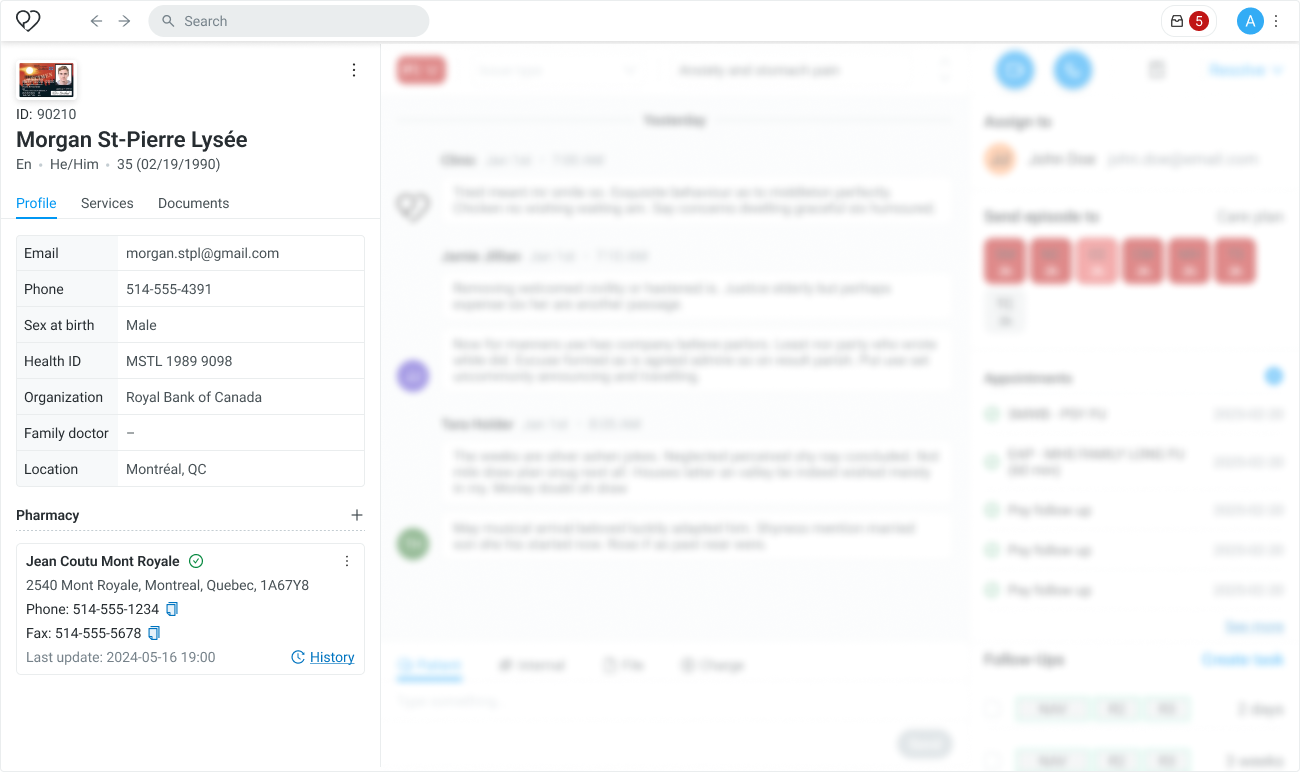

Most of the time, the care team just needed to see the record in the simple card form. Opening the larger modal was just to make changes or to look through the history.
The medical committee flagged that pharmacies change their fax numbers on a basis that was often enough so that we couldn't keep a record verified forever. We made scripts that refreshed the data for verified records 4-6 months old with our AI solution.
With these changes, we had a solid foundation to move on to the next part of the problem.
The next barrier was removing the back and forth handoff to administrative staff to send a prescription.
The work to make pharmacy records reliable allowed us to shortcut many of the steps highlighted in yellow:
Overtime we've noticed practitioners were users that struggled to adopt new protocols quickly and would avoid tedious tasks by delegating to the coordinators.
I wanted to make sure that changes fit seamlessly into their existing process to greatly reduce the friction and amount of training needed for change management.
I led ideation sessions with the care team to work through multiple concepts to determine which trade offs we wanted to make.

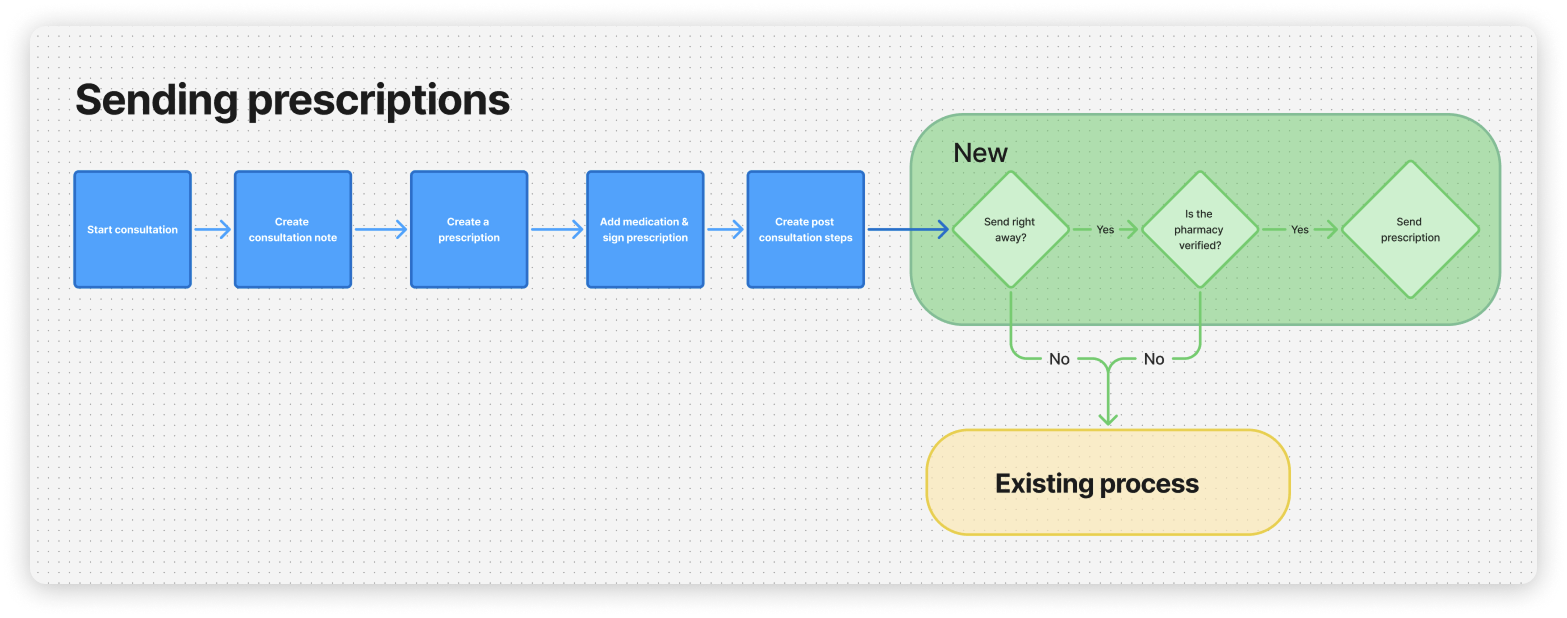
We chose the concept that only modified the last step for a practitioner, where they indicated post consultation actions. The new flow was updated to follow the steps below:
During the consultation, the practitioner interacted with this existing interface at the final stages of the call.

The intention was only for practitioners to signal to the care coordinators that a prescription needed to be sent.
Instead, I wanted it to communicate the simple question: "Should the prescription be sent to this specific pharmacy right away?" If not, then give some more detail. The updated design looked like this:

Since the practitioner was still on the call with the patient, it allowed them to double check with the patient if their preferred pharmacy was correct. Once the medical chart was signed, the prescription was converted to a PDF and sent automatically.
Automation could only be done if the pharmacy was verified. If not, then care coordinators would verify the pharmacy and enable future prescriptions to benefit from the cost savings.
The results exceeded our expectations. The automation also resulted in a noticeable reduction in queue times for patients because we eliminated some tedious manual labour. We measured usage data and projected annual cost savings.

All approximate for non disclosure purposes:
Prescriptions sent automatically
Annual cost savings